Early detection and treatment of eye issues can help prevent significant vision loss. See your doctor immediately if you notice any changes like blurry vision, floaters, flashing lights, any pain or pressure in your eyes, or sudden loss of vision.
Familiarize yourself with symptoms of common eye problems.
Monitor your vision regularly for any changes or new symptoms.
Report any concerns or sudden changes to your healthcare provider promptly.
Schedule additional eye exams if needed to track any ongoing issues.
Remember to Blink
When focused on digital devices or other intricate visual tasks, we forget to blink, causing our eyes to dry out. Dryness can be a significant issue for people with diabetes, leading to discomfort and potential eye complications. Make it a habit to blink regularly, especially when using digital devices.
Use the 20-20-20 rule: take a break every 20 minutes, and look at something 20 feet away for 20 seconds.
Remind yourself to blink more frequently during visually demanding tasks.
Consider using a timer or app to remind you to take breaks and blink.
Stay Hydrated
Good hydration is critical for overall health and eye health. People with diabetes may also be at risk of dry eyes. Consuming ample liquids can help keep your eyes lubricated and healthy.
Drink at least eight 8-ounce glasses of water per day, or as recommended by your healthcare provider.
Consume water-rich fruits and vegetables like watermelon, cucumber, oranges, and tomatoes.
Avoid excessive caffeine, alcohol, and high-sugar beverages, which can lead to dehydration.
Treatment Options for Diabetic Eye Complications
In managing diabetic eye complications, prompt diagnosis and treatment can prevent or slow down the progression of vision loss. Here are the general treatment options available:
Laser Therapy
Laser therapy, also known as photocoagulation, is primarily used in the treatment of Diabetic Retinopathy and Diabetic Macular Edema. There are two types:
Focal Laser Treatment: This slows the leakage of blood and fluid in the eye. It's done in a single session, where leaks from abnormal blood vessels are treated.
Scatter (Pan Retinal) Laser Treatment: This shrinks the abnormal blood vessels and generally requires two or more sessions.
Intravitreal Injections
Intravitreal injections are used to deliver medication directly into the eyes to treat conditions such as Diabetic Macular Edema and Proliferative Diabetic Retinopathy. Medications used often fall into one of the following categories:
Anti-Vascular Endothelial Growth Factor (Anti-VEGF): These drugs block the actions of a protein that can cause abnormal blood vessels to grow and leak fluid, causing the retina to swell and vision to decrease.
Corticosteroids: Steroid medications can reduce inflammation and decrease the swelling of the retina.
Medications
Oral or injected medications can help control blood sugar levels, blood pressure, and cholesterol levels, thus slowing down the development or progression of diabetic eye complications.
Surgery
Surgery may be necessary in advanced stages of diabetic eye disease, particularly if there is significant bleeding into the eye (vitreous hemorrhage) or if retinal detachment occurs. Procedures can include:
Vitrectomy: This surgical procedure involves the removal of the vitreous gel to clear away blood from leaking vessels.
Retinal Detachment Surgery: If the retina has detached, surgery involving laser, freeze treatment (cryotherapy), or gas bubble (pneumatic retinopexy) may be necessary to reattach it.
Conclusion
In conclusion, maintaining a rigorous eye care regimen is of paramount importance for people with diabetes. It's essential to understand that safeguarding your sight goes way beyond that standard yearly eye checkup. Embrace these tips in your routine to maintain the healthiest eyes possible, even in the face of diabetes. By staying vigilant about your vision, you're not just looking out for your eyes, but you're also safeguarding your quality of life.

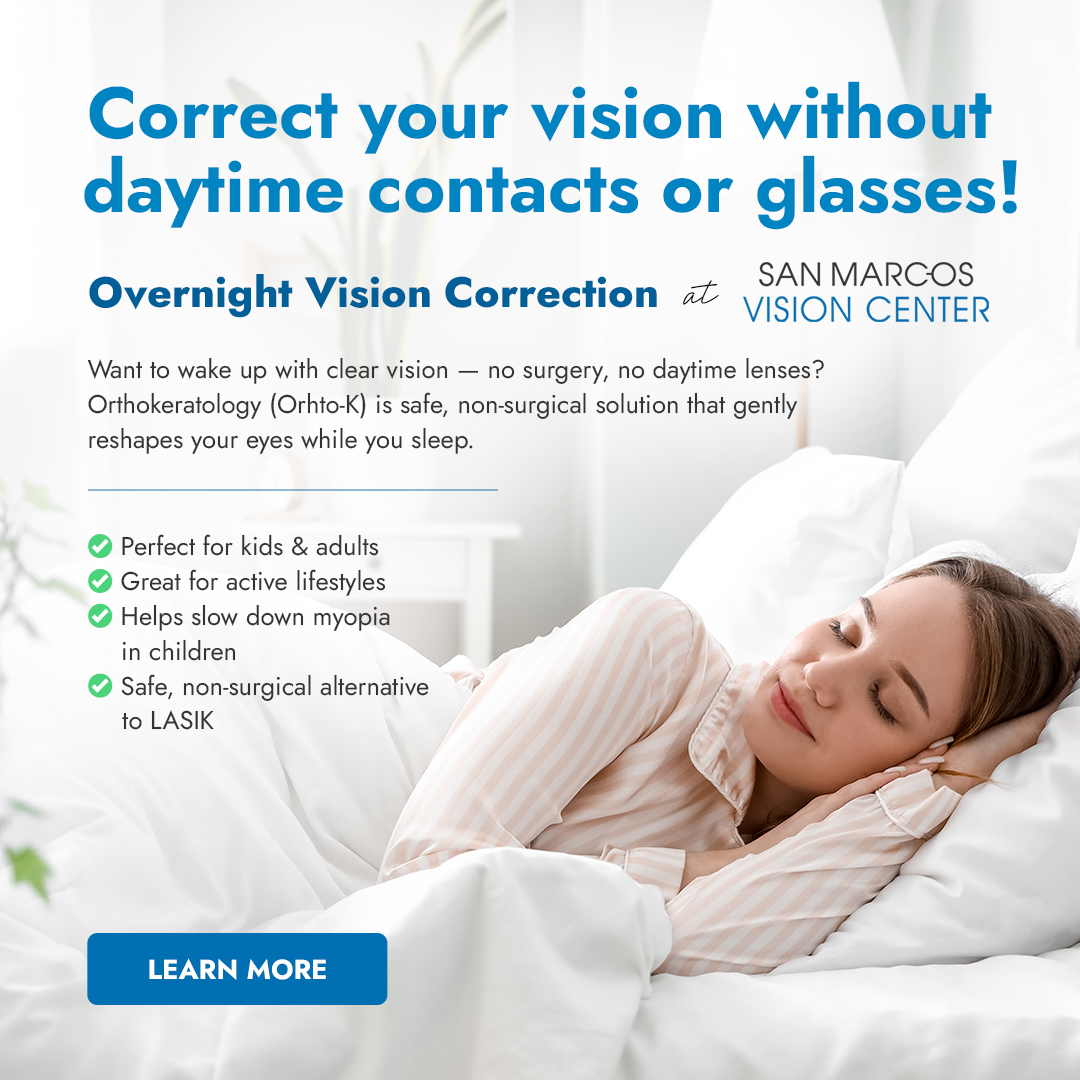
 Specialty Contacts
Specialty Contacts